As U.S. schools resume in-person learning this fall, parents and administrators may have to deal with more outbreaks of colds and other seasonal respiratory illnesses than usual. If so, these outbreaks aren’t likely to be especially dangerous for school-age children, but could be problematic for traditionally more vulnerable younger siblings or elderly relatives, experts say. And because the symptoms of these illnesses often mirror those of COVID-19, it could make having kids back in the classroom — and keeping them there — that much more challenging.
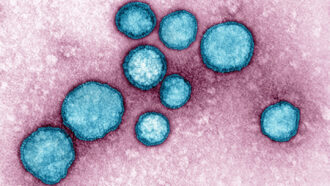
Respiratory viruses, which cause common colds and the flu, typically circulate in colder months. But last year’s cold-and-flu season was practically nonexistent. Some cold-causing viruses, such as rhinoviruses and enteroviruses, kept spreading, though at reduced levels. Influenza and respiratory syncytial virus, or RSV, however, were held to historically low levels, an unintended effect of COVID-19 pandemic precautions such as border closings, wearing masks and social distancing (SN: 2/2/21). Other respiratory pathogens that cause cold-like symptoms, such as adenoviruses and parainfluenza viruses, also had very mild seasons last winter, researchers with the U.S. Centers for Disease Control and Prevention report July 23 in Morbidity and Mortality Weekly Report.
“There’s been a huge, huge change during the COVID pandemic in the circulation of what we think of as the commonplace respiratory viruses and the seasonal respiratory viruses,” says Ellen Foxman, an immunologist at Yale School of Medicine. RSV and flu “have virtually disappeared during the COVID pandemic, almost certainly because of the mitigation measures.”
But, worryingly, that absence has created a larger-than-usual population of people vulnerable to these common respiratory viruses. When people don’t get sick with the viruses for a year or two, immunity to them wanes. That makes those people, including school-age kids, more likely to get sick in the coming months.
Keeping COVID-19 precautions such as wearing masks in place could help keep these other respiratory viruses from surging. Without those precautions this coming winter, experts think high rates of RSV and other common respiratory viruses are probable.
A string of endless colds would be annoying and possibly disruptive to schooling, given that these viruses often cause symptoms like runny noses and cough, similar to some COVID-19 symptoms. That means kids might have to miss school while waiting for COVID-19 test results. What’s more, these kids can pass these infections on to very young or elderly family members.
“The kids are going to go to school, they’ll bring it home to the family and the younger children,” says Ian Barr, a virologist at the World Health Organization’s Collaborating Centre for Reference and Research on Influenza at the Doherty Institute in Melbourne, Australia. Those family members “are the ones who will … end up with the symptomatic and in some cases, serious infections.”
Influenza and RSV are the most serious seasonal respiratory viruses, especially for the very young and the elderly. The CDC estimates that RSV typically puts about 58,000 children under age 5 in the hospital each year and is the most common cause of pneumonia in children under a year old. It also hospitalizes more than 177,000 adults 65 and older. Influenza viruses typically kill around 36,000 people a year in the United States and hospitalize almost half a million, the CDC estimates.
With the pandemic-induced lull in these diseases, there is now a larger population of people vulnerable to RSV and that has led to unusual, off-season outbreaks of the illness in some places, researchers report July 22 in Eurosurveillance. Multiple states in Australia saw off-season RSV peaks in summer months that were even larger than traditional winter peaks. In Western Australia, the normal cold-weather peak for RSV is a little over 40 detections per week in the middle of July. But in 2020, there was no cold-weather peak. RSV infections stayed low until the warm months, and then peaked at over 100 detections a week in December, researchers reported in February in Clinical Infectious Diseases.
In the United States, detections of RSV have been mostly rising since spring, according to the CDC’s National Respiratory and Enteric Virus Surveillance System. In late March, there were about 100 detections a week in the surveillance system. In the week ending July 24, there were more than 3,100 weekly detections. That’s still far below a normal RSV season; for example, cases peaked at 24,280 detections a week in December of 2019. But the timing is the thing, experts say. “It’s rare for most of these respiratory diseases to be circulating in summer,” says Barr, a coauthor of the Eurosurveillance study.
Short and sharp summer outbreaks of RSV — like those seen in Western Australia in December of 2020 — seem to lead to a lower surge later, Barr says. But places where levels of RSV and other seasonal respiratory viruses stay low through the warm months, could turn into hot spots in the fall and winter with a larger-than-normal season.
There is one big exception to that prediction: If the coronavirus is widespread during winter, “it may still keep these other viruses low,” says Richard Webby, a virologist at St. Jude Children’s Research Hospital in Memphis, Tenn.
If so, that wouldn’t just be because of COVID-19 precautions left in place to help control the coronavirus. At play would also be a phenomenon called viral interference — when one respiratory virus dampens the spread of other viruses (SN: 9/18/20). There are two ways that this can happen: by sickening people and having them stay home — removing them from the population than can be infected at a given school or workplace — or by directly priming infected individuals’ immune system to fight off other viral infections.
“When one virus is there, there’s a heightened state of general antiviral defenses” in the body, Foxman says. “So you would predict that for a certain … period after somebody has one viral infection, they may be more resistant to getting another viral infection.” Still, this scenario would mean relatively high levels of coronavirus cases in the country — not exactly something to hope for.
“If [I] had to guess what was going to happen, [I’d say] that some of these other respiratory diseases are going to be more of a problem than influenza when your kids go back to school,” Barr says. “The parainfluenzas, the adenoviruses, RSV — these sorts of viruses are more likely to circulate than influenza.”
That’s partly because the flu vaccine exists, which can help lessen influenza outbreaks. And it’s partly because of the way that the flu spreads and evolves as it moves around the world, experts say, and how that spread seems to be more affected by border closures and reduced travel than other respiratory viruses. Less travel around the world in the last two years has prevented influenza epidemics from spreading out of countries to other places, and the flu remains at very low levels worldwide.
Ultimately, “it’s a little hard to predict what’s going to happen, because we have never had this kind of disruption before in the transmission of these viruses,” Foxman says. “But of course, it’s very interesting to follow it and important to see what happens, because we’re going to learn a lot.”


