For millions of people, COVID-19 doesn’t end with a negative test. Weeks or months after traces of the virus disappear from noses and throats, symptoms can persist or come back. New ones might pop up and stick around for months. People suffering from long COVID are unwillingly in it for the long haul — and it’s still unclear who’s at the highest risk for the condition.
Researchers don’t yet have an official definition for long COVID, and its symptoms are wide-ranging (SN: 7/29/22). Some people struggle with extreme fatigue that interferes with their daily lives. Others can’t concentrate or struggle with memory amid thick brain fog. Still others have organ damage or a persistent cough and difficulty breathing.
“There are a variety of different kinds of ways that people can have long COVID. It’s not just the one thing,” says Leora Horwitz, an internal medicine physician at New York University Langone Health. “That’s what makes it so hard to study.”
This spectrum of symptoms makes pinning down who’s at high risk for long-term health problems from the disease especially hard. Some post-COVID conditions may stem from virus-induced damage or from the stress of being hospitalized with severe disease. In other cases, the body’s own immune response to the virus could drive the damage. Or the virus may be hiding somewhere in the body, possibly the gut, helping symptoms to persist (SN: 11/24/20). Different causes may have different risk groups, says Hannah Davis, cofounder of the Patient-Led Research Collaborative, a research and advocacy group studying long COVID.
There are some broad hints about who’s at risk. Studies suggest that women are more likely than men to have lingering symptoms. COVID-19 patients with more than five symptoms in the first week of infection or preexisting health conditions such as asthma may be more likely to develop long COVID. Age also appears to be a risk factor, though results are mixed regarding whether the burden falls on older people or middle-aged people. Populations that were disproportionally hit by COVID-19 overall — including Black and Hispanic people — may similarly face disparities for long COVID. And while vaccination seems to protect people from developing long COVID, Horwitz says, it’s still unclear by how much.
Age is a risk factor for severe COVID-19, and the U.S. Centers for Disease Control and Prevention lists more than 30 health problems, including cancer and lung disease, that also raise the risk. “So many researchers assume that those [risk factors] will be the same for long COVID and there’s no scientific basis for that,” Davis says. There are many more that researchers could be missing when it comes to long COVID.
Using health records and exams, and knowledge of ailments with symptoms similar to long COVID, experts are on the hunt for those risk factors.
Examining health
When it comes to getting a better handle on who’s at risk for long COVID — which also goes by the wonky alias Post-Acute Sequelae of SARS-CoV-2 infection — electronic health records may hold important clues.
Horwitz is part of the U.S. National Institutes of Health’s RECOVER initiative that aims to understand the long-term impacts of COVID-19. One arm of the study involves mining millions of electronic health records to find potential patterns.
Studying millions of these records should pinpoint potential risk factors that are rare in the population overall but perhaps more common for people with long COVID, Horwitz says. “That’s hard even in a cohort study of thousands.”
But health records aren’t perfect: They depend on physicians logging that patients are having trouble sleeping or focusing, or that they’re exhausted. “The things people are complaining about, we’re really bad at writing down those diagnoses on the record,” Horwitz says. “So we miss that.”
To account for health records’ deficiencies, Horowitz and colleagues are also directly studying thousands of people. Participants answer a questionnaire every three months so that the team can identify what kinds of symptoms people have and whether they’re getting better or worse.
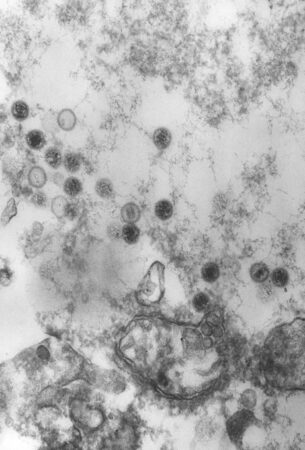
Then blood, urine, stool and saliva samples can reveal what’s happening in the body. Tests on those samples can uncover if the coronavirus is still around and causing trouble, or if the immune system has learned to attack the body itself. Participants with abnormal test results will undergo additional, targeted testing.
“Unlike electronic health records where it’s hit or miss, like somebody might have had a CAT scan or might not, here we say, ‘OK, you have trouble breathing. We will take a look at your lungs,’” Horwitz says.
The study includes a range of participants: adults and kids, pregnant people, those currently with COVID-19 and people who died after having the disease.
Some of the potential risk factors that the team is looking for include autoimmune diseases and other viral infections. The list may grow as more people join the study. “We’re trying to balance the fishing versus making sure that we’re at least fishing for things that could be in the water,” Horwitz says.
Among short supply, though, are people who never caught the virus — important “controls” to highlight what’s different about people who got COVID-19.
So far, more than 7,000 people have signed up, and the group plans to recruit around 10,000 more. It’s a lot of data, but early results may soon start coming in.
“We’ll probably try to do an interim peek at those data this fall,” Horwitz says. “It’s tricky because we deliberately wanted to enroll 18,000 people so we would have enough power to really look at the things we care about. I don’t want to cheat and look too early, but we also know that there’s a lot of interest.”
Striking similarities
Some long COVID symptoms — brain fog, fatigue and trouble sleeping — mirror another illness: myalgic encephalomyelitis/chronic fatigue syndrome, or ME/CFS. Other long COVID symptoms, such as rapid heartbeat and dizziness, fall in the category of nervous system disorders called dysautonomia. Similar symptoms could belie similar risk factors.
Yet potential risk factors for those conditions are largely missing from long COVID research, says Davis, who has had long COVID since March 2020. Among the possibilities that scientists are considering are things like Epstein-Barr virus, migraines and some autoimmune diseases.
Epstein-Barr virus could be a big one, Davis says. Infections last a lifetime because the virus can go into hiding in the body and possibly reemerge. That virus has been linked to ME/CFS for decades, though the connection is tenuous, Davis says.
Some early hints of a link between Epstein-Barr virus and long COVID already exist. Multiple studies have found evidence in blood samples from some long COVID patients that the immune system recently battled with Epstein-Barr virus, which can cause infectious mononucleosis, a disease characterized by extreme fatigue. Other studies have found signs of the virus itself. And in 2021, Davis and colleagues found that 40 out of 580 people with symptoms of long COVID who responded to an online survey reported having a current or recent Epstein-Barr virus infection.
With ME/CFS, it’s possible that another illness caused by a different virus triggers the Epstein-Barr virus, which then causes the fatigue syndrome. Given the parallels between that condition and long COVID, some scientists are wondering if the two are actually the same disease, with the coronavirus now known as one trigger.
Examining health conditions that raise the chances of long COVID could provide answers for both diseases, says Nancy Klimas, an immunologist at Nova Southeastern University in Fort Lauderdale, Fla. That’s in part because researchers can more easily identify people who developed lingering symptoms after a bout of COVID-19 compared with unknown infections that may precede ME/CFS.
Also, “there’s a huge difference in these two fields and it’s money,” Klimas says. She now has funding from the CDC to compare long COVID patients with people who have ME/CFS. The team hopes that physical exams and specialized tests will reveal whether the two diseases are indeed the same and be a step toward understanding the mechanisms behind the lingering symptoms.
Still, since long COVID as a whole encompasses such a wide range of symptoms, it will take time to uncover who is at risk of what.
If COVID-19 were just one disease impacting the lungs, heart or brain, the research might be easier, Horwitz says. “But we have to test everything.”